Skin Cancer Treatment
What is a Skin Cancer?
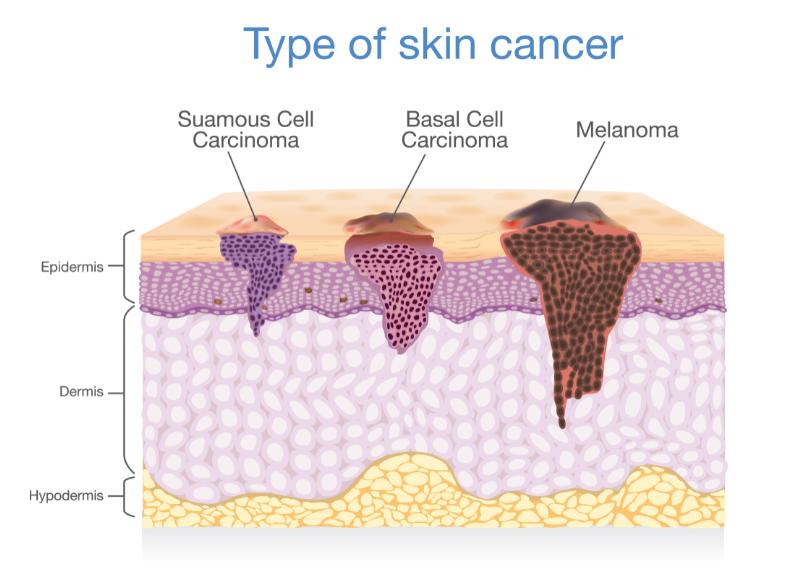
Skin cancer is an abnormal proliferation of skin cells that forms a skin growth. Most skin cancers develop due to over exposure to the sun, however the sun alone is not the sole factor. Genetics are undoubtedly count for a huge reason why some patients develop skin cancers and others do not. The three major types of skin cancer are basal cell carcinoma, squamous cell carcinoma and melanoma. Dr. Michele Green is an expert in diagnosing and treating all forms of skin cancer. As chief resident in dermatology at the Mount Sinai School of medicine in NYC, she has always had a keen interest in skin cancer prevention and detection. As a resident, Dr. Green studied with the brilliant Dr. A. Bernard Ackerman and researched the surgical margins needed to treat skin cancers such as malignant melanoma. It is with this eye on prevention, detection, and treatment, that Dr. Green begins each new patient exam with a complete skin examination, even when the focus may be a cosmetic consultation.
Skin Cancer Detection
When it comes to skin cancer, early detection plus prompt diagnosis and the right skin cancer treatment is the best combination for recovery. Although careful protection of your skin from the sun is the best prevention, skin cancer can also develop in areas of the skin that aren’t regularly exposed to sunlight. A thorough skin evaluation from Dr. Michele Green, voted one of NYC’s best dermatologists, establishes the necessary baseline for patients to better gauge their skin health.
Skin cancers falls into three basic cancer types: basal cell carcinoma, squamous cell carcinoma and melanoma. Understanding which type of skin cancer you have will better determine your course of treatment. Treating precancerous skin lesions is also part of a comprehensive skin cancer treatment plan.
Actinic Keratoses (Pre-cancers)
An actinic keratosis is a scaly or crusty lesion that can sometimes go unnoticed. More than ten million Americans have actinic keratoses, making it the most common pre-cancer. Individuals who have a fair complexion and spend time in the sun are at a greater risk for developing actinic keratoses. If left untreated, these lesions can lead to squamous cell carcinoma. Approximately ten percent of actinic keratoses advance to squamous cell carcinomas, and approximately forty to sixty percent of squamous cell carcinomas begin as an untreated actinic keratoses.
Once an actinic keratosis is identified, there are many treatment options, including topical medications such as Efudex, Carac, and more comprehensive treatments such as Photodynamic Therapy (PDT). Dr. Green will determine the severity of your lesions and choose the best method of treatment for your skin.

Squamous Cell Carcinoma
According to the American Cancer Society Squamous Cell Carcinoma (SCC) is the second most common skin cancer with 700,000 new cases diagnosed each year. People who have fair skin tone or who exposed to the sun for long periods of time have a higher chance of developing squamous cell skin cancers during their lifetime. Recurrent use of tanning beds also puts one at risk for developing squamous cell cancers. Individuals who use tanning beds are 2.5 times more likely to develop squamous cell carcinomas than individuals that do not use tanning beds.
Various pre-cancers or pre-cancerous growths, such as the Human Papillomavirus (HPV), may evolve into squamous cell carcinomas. If left untreated, squamous cell carcinoma may spread to other organs and become deadly. Approximately 2,500 deaths each year are caused by untreated squamous cell carcinomas. Early detection is important, since once identified, squamous cell carcinoma is entirely treatable. Dr. Green recommends various methods to treat squamous cell carcinomas including excisions, electrodessication and Moh’s surgery.
Basal Cell Carcinoma
Basal Cell Carcinoma is the most common skin cancer that affects approximately two million people each year. The majority of basal cell carcinomas occur on areas of the skin that receive the most sun exposure, such as the face, neck, back, and scalp. Even though basal cell carcinoma rarely spreads to other organs, it may harm surrounding healthy skin tissue through local invasion, which is why early detection and treatment are important. Early stages of basal cell carcinomas are easily treated with various methods. When a basal bell carcinoma is diagnosed by Dr. Green, treatment is either by excision, Moh’s surgery or electrodessication, depending on the size and anatomic location.
Basal cell carcinoma is a type of skin cancer which forms within the basal skin cells. The basal cells are responsible for the regeneration of new skin cells as old cells die.
Basal cell carcinomas presents as a lesion or skin growth that does not heal. In addition, the skin growth usually presents with the following characteristics:
- A pearly white, flesh colored or pink bump that is translucent with visible blood vessels which can rupture leaving a wound that does not heal. These types of basal cell carcinoma are most common and generally appear on the face and ears.
- A brown, black or blue or dark growth slightly raised with a translucent edge.
- A flat, scaly, reddish patch which presents on the back or chest with a raised and propensity to grow quite large.
- Morpheaform basal cell carcinoma is the least common type it is a white, waxy, scar-like lesion with ill-defined borders.
According to the American Cancer Society approximately 5.4 million basal and squamous cell skin cancers are diagnosed in the United States each year.
Melanoma
Melanoma is one of the most serious type of skin cancer which develops in the skin cells (melanocytes) that produce melanin. Melanin is the pigment that gives your skin its unique color. While melanoma is most common of the serious skin cancers there are other less common serious skin cancers such as Merkel Cell Carcinoma. Melanoma can form anywhere on the body including the eyes. In patients with darker skin tones, in African American and Asian individuals, melanoma can form on the soles of the feet, palms and nail bed.
It is not known exactly how melanomas are formed but overexposure to the sun and man made light such as tanning beds does increase your risk of developing a melanoma. Genetics play a part as well as malignant melanomas often run in families.
According to the American Academy of Dermatology skin cancer is the most common form of cancer in the United States. Your risk of developing a melanoma doubles if you have had 5 or more sunburns, and a single childhood burn doubles your lifetime risk for melanoma . In addition, current statistics show that one in five Americans will develop a skin cancer in their lifetime. While melanoma is the least common form of skin cancer it is the most lethal accounting for 1% of all skin cancers.
Proper sun precaution while outdoors such as wearing sunscreen and sun protective clothing is important to protect the skin from sun damage. Also, diligent follow up visits to your dermatologist, like Dr. Green, are important for skin examinations to detect the earliest signs of skin cancer.

Early detection of Melanoma Skin Cancer
It is critical to understand the ABCDEs of malignant melanoma in order to provide early detection and treatment of this life threatening skin cancer.
A – Asymmetry: One half of the lesion doesn’t match the appearance of the other half.
B – Border irregularity: The edges are uneven, notched, or blurred.
C – Color: The color or pigmentation is not uniform throughout. There are shades of tan, brown, or black or even blue, red, and white present.
D – Diameter: The size of the mole is greater than ¼ inch (6mm) which is about the size of a pencil’s eraser. There are melanomas which are first developing which are even smaller in size.
E – Evolution: There is a change in the size, shape, symptoms (such as itching or tenderness, or color of the mole, or surface (bleeding) of the mole.
If you notice any of these symptoms, please consult Dr. Michele Green for an examination of the mole and have a complete skin exam performed.
Stages of Melanoma
The TNM staging system developed by the American Joint Committee on Cancer (AJCC) was created to score the stages of a melanoma. According to the model each letter of the system is a contributing factor in the staging the tumor. The “T” stands for tumor and ranks the tumor based upon size from 0- to 4. Each number indicates the size of the tumor -0- being a superficial melanoma or melanoma in situ (the cancerous tissue has only penetrated the epidermis) to stage 4 which means the cancer has metastasized beyond the tumor into the lymph nodes or other organs.
N represents the lymph nodes and identifying if the cancer has spread to the lymph nodes. Cancer that has spread to the lymph nodes is more serious and requires more aggressive treatment.
M identifies whether the cancer has metastasized or not. In addition to TNM staging model diagnostic testing such as ultrasound, and blood tests to check liver functions and lactate dehydrogenase (LDH) levels are also performed to complete the staging of the melanoma.
Risk factors for skin cancer
The following factors may increase your risk of skin cancer and the type of cancer:
Chronic sun exposure is the number one reason why patients develop skin cancer. Chronic exposure to the sun is one of the leading causes of skin cancer. In addition, a history of severe sunburns also severely increases your risk of skin cancer.
Radiation therapy-There is an increased risk of developing basal cell carcinomas and squamous cell carcinomas if you have had previous radiation treatments.
Fair skin- The risk of skin cancer is higher for individuals with less melanin. If you have light colored eyes, and burn easily from sun exposure with the propensity to freckle, you are at a higher risk of developing a skin cancer.
Increasing age- Your risk of skin cancer increases with age as most skin cancers arise from years of cumulative sun exposure. As you get older, the likelihood for developing skin cancers rises. Younger individuals can also develop skin cancer due to their exposure to UV light , tanning beds, and genetic pre-disposition.
A personal or family history of skin cancer- If you’ve had basal cell carcinoma one or more times, you have a good chance of developing it again. If you have a family history of skin cancer, you may have an increased risk of developing basal cell carcinoma. In particular, a family history of melanoma makes you much more likely to develop a malignant melanoma.
Immunotherapy – Immune suppressing medications can increase your risk of developing skin cancer.
Skin cancer treatment options
The goal of any skin cancer treatment is to remove the cancer completely. The best treatment depends on the type of skin cancer, location, and size. The treatment selected is also dependent on whether this is a recurrence of this skin cancer. While most skin cancers are treated and managed by dermatologists, in some cases you may need to consult an oncologist. This is especially true in cases of malignant melanoma or skin cancers that are deep or have metastasized to other organs or lymph nodes.
Surgery
Squamous cell carcinomas with high probability of reccurrence, Basal cell carcinomas and Melanomas are most often treated with surgery to ensure removal of all the cancerous cells.
Surgical treatment options include:
Excision – This treatment option is usually used to treat basal cell carcinoma and melanomas. During the procedure the area anesthetized and a skin biopsy of the cancerous lesion is excised. The tissue sample is sent to a dermatopathologist who examines the sample under a microscope to be sure all the cancerous cells have been removed and there is no remaining cancer.
Mohs surgery – Mohs micrographic surgery involves removal of abnormal cells one layer at a time. During the procedure a pathologist reviews each layer of tissue sample removed and examines it under a microscope. This process is repeated until there are no cancerous cells only normal tissue is seen. This process is very thorough and allows the surgeon certainty that all the abnormal cells is removed.
Mohs surgery is usually recommended for basal cell carcinoma with a high risk of reoccurrence and melanoma.
Other Skin Cancer treatments
Your doctor may recommend other non surgical treatments if surgery is not an option.
Other treatments include:
Photodynamic therapy – Photodynamic (PDT) therapy is a combination of photosensitizing drugs and blue light to treat superficial skin cancers such as actinic keratoses. The procedure involves a topical application of a photosensitizing medication, called Levulan, which causes the cancer cells to become activated and treated with the blue light.
Curettage and electrodesiccation – This treatment involves scraping the surface of the lesion with a curette and using a hyfrecator to destroy the rest of the lesion. This treatment option is best for superficial skin cancers and lesions with low probability of reccurrence.
Radiation therapy – Radiation therapy uses high-energy laser beam similar to X-rays to kill cancerous cells. Radiation is often used after Melanoma skin cancer treatment when there is an increased risk of reccurrence. It can also be done on parts of the body for basal cell carcinomas or squamous cell carcinomas when surgical excision is not an option.
Cryosurgery – This treatment entails freezing cancerous cells with liquid nitrogen. Freezing is usually a treatment option for treating superficial lesions such as actinic keratosis and some squamous cell carcinomas. The treatment It may be done after curettage and electrodessication to prevent recurrence.
Topical treatments – There are four FDA approved topical prescription creams that can be considered for treating skin cancers when surgery is not an option. The four creams are Fluorouracil (Efudex), Imiquimod (Aldara), Diclofenac (Solaraze) and Ingenol mebutate (Picato). Actinic keratoses can be treated with all four of these topicals creams. However, other types of skin cancers may need additional therapies.
Basal cell carcinomas can also be treated with topicals such as fluorouracil which is a chemotherapeutic drug which works by interrupting cell division within the basal cell causing the cancerous cells to die. This treatment is used only for superficial and low risk basal cells carcinomas.
Diclofenac is an anti-inflammatory non-steroidal drug mainly used to treat actinic keratoses. The mechanism of action for Imiquimod is that it is used to treat actinic keratoses and basal cell carcinomas via immune system. The drug triggers an immune response to react and destroy the skin cancers.
Clinical trials for skin cancer
Clinical trials allow doctors the ability to make scientific advances through voluntary participation and research. These clinical trials allow dermatologists the ability to find more successful ways to manage and treat non-melanoma skin cancers and keratinocytic lesions. Most cancer research focus on new and effective therapies to treat existing conditions. The studies evaluate new surgical approaches, treatment combinations, new drugs, symptoms and side effects. In order to get FDA approval, companies must submit clinical trials for medications, medical devices and procedures to the for review and approval before they are made available to the general public.
If you’re concerned about new or changing moles and worried that it is skin cancer, it’s time to schedule a complete skin exam with Dr. Green. Contact us online today or call 212-535-3088 to learn more about Dr. Green’s comprehensive approach toward skin cancer prevention, detection and treatment.
 212-535-3088
212-535-3088